 |
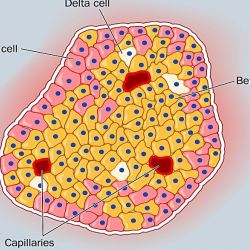
Pancreatic Islet Cells Image: Medscape
|
As time goes by, their discovery becomes less surprising. This is because the role of infectious pathogens in causing secondary disease is now well established, and will almost certainly grow. The importance of these discoveries cannot be overstated. Every time a pathogen is attributed to a disease or condition, it opens up a new avenue for treating that condition.
For example, the following viruses are now known to cause different cancers:
- Hepatitis B - liver
- Hepatitis C - liver
- Human papillomavirus (HPV) - cervix, anus, oral cavity
- Human herpesvirus-8 - Kaposi sarcoma
- Epstein Barr - Burkitt's lymphoma
- Human T-lymphotrophic virus-1 (HTLV-1) - leukemia and non-Hodgkin lymphoma
This list will almost certainly grow as associations between pathogens and seemingly unrelated diseases, especially autoimmune conditions, unfold. Alzheimer's Disease is one example. Although beta-amaloid plaques are clearly associated with the development of AD, it is unclear whether the plaques are the cause of the disease or the result of it. The possibility of viral (HSV-1) or bacterial infections (chlamydia or spirochetes) being the cause of AD has been been raised recently. Assuming that this hypothesis it correct, it may be possible to prevent AD by treating the underlying infection—something that is crucial because despite the enormous amount of resources thrown at, there has been absolutely no progress made in either preventing or modifying the disease.
The idea that type 1 diabetes (T1D)—also called insulin-dependent diabetes mellitus, or IDDM— (1) may be a result of a malfunction of the immune system from its response to the pathogen is not new. Anecdotes about children developing the disease following an infection are common. Although its cause remains unknown, T1D is increasingly being seen as an autoimmune disorder. In this case, the immune system attacking insulin-producing beta cells in the pancreas. Now, there is more evidence to support the pathogen theory.
A new study, which was published in Diabetologia, (the journal of the European Association for the Study of Diabetes) offers additional support for the T1D-pathogen theory, courtesy of Dr. Hanna Honkanen and colleagues at the University of Tampere in Finland. The group examined stool samples from two groups of children: those who tested positive for pancreatic islet antibodies and those who demonstrated antibodies only for enterovirus (the control group). There was a strong correlation between T1D and enterovirus (2).
In the control group of 282 children, 169 tested positive for enterovirus. But, of the 129 children who tested positive for islet antibodies, 108 of them later developed enterovirus infections. In other words, the children who had T1D were found to have three times more enterovirus infections than children who did not.
The authors discussed the strength of the study:
"The present study suggests that enterovirus infections in young children are associated with the appearance of islet autoantibodies with a time lag of about 1 year. This finding supports previous observations from other prospective studies suggesting that enterovirus infections may play a role in the initiation of the beta cell-damaging process.Dr. Hanna Honkanen in Diabetologia, January 9, 2017
The weaknesses include the facts that the results were from only one country, and that respiratory samples, which could have detected other enteroviruses that were not detected in the stool were not taken.
The implications of these findings are compelling - raising the possibility of developing vaccines that would prevent T1D, which would be a groundbreaking development.
Notes:
(1) Type 1 diabetes (insufficient production of insulin) accounts for only 5% of all cases. Type 2 accounts for the rest. People with T2D have plenty of insulin (sometimes too much), but the insulin does not function properly. Insulin resistance is the hallmark of T2D.
(2) Enteroviruses are a huge family (dozens) of RNA viruses. Enteroviruses are ubiquitous. While some of them are associated with human disease, most produce no symptoms. Examples of disease causing enteroviruses include polio (poliovirus), viral heart infections and hand-foot-and-mouth disease (Coxsackievirus), and a cold-like respiratory infection, mostly in children (Enterovirus D68). There are no vaccine to prevent any enterovirus infection, nor are there any drugs to treat them.
No comments:
Post a Comment